Surgical Techniques: Flap vs. Flapless
Overview:
- Ultimately, the choice of flap vs flapless comes down to doctor preference and clinical indications on a case-by-case basis.
- We will look at which situations indicate a flapless procedure, if the patient is a candidate for flapless, and the surgical protocol.
- Both techniques have advantages and disadvantages. Both techniques benefit significantly from the use of pre-operative CBCT imaging.
- We will discuss flap techniques both in designing the shape of the flap and incisions, as well as surgical tips and techniques.
- As we will address in the article, the patient’s bone quantity and quality will be a key factor when determining protocol.
Q. Should I consider a flapless technique for my case?
When considering a flapless versus traditional flap technique, dentists should compare the advantages and disadvantages of a flapless technique.
| When applicable to your case, a flapless procedure has many benefits: |
|---|
| + Eliminates need for sutures and suture removal |
| + Reduces tissue trauma |
| + Reduces bone absorption |
| + Reduces surgical time |
| + Reduces risk for complications related to tissue manipulation (swelling, hemorrhage, morbidity) |
| + Increases patient comfort |
| + Positive perception to the patient (minimally-invasive) |
| With comparatively fewer disadvantages: |
|---|
| - Lack of subsurface visibility of bone and anatomical structures* |
| - Limits manipulation of hard/soft tissues |
| - Limits irrigation effectiveness |
* Note that the difficulties associated with a lack of visibility of bone and anatomical structures may be significantly reduced with CBCT imaging.
However, as not all patients will be candidates for flapless, clinical judgement must be used to determine viability on a case-by-case basis. Generally, qualifying patients will have well-healed gingiva and adequate bone dimensions to hold an implant, without the need for prior bone reduction or grafting. I recommend assessing bone quantity and quality with CBCT imaging evaluation for the most accurate results. Qualifying patients will also need to retain at least 2mm of attached gingival tissue surrounding the intended surgical site after making the ~4.9-6.4mm diameter incision.
.png)
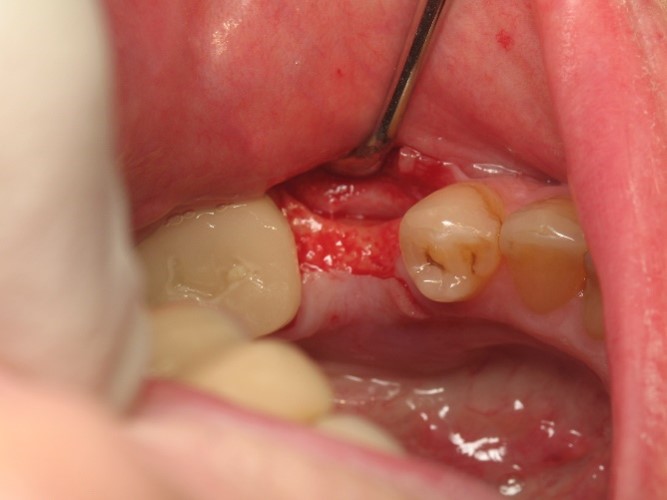
A flapless procedure may be contraindicated for patients that have had recent extractions within a year, as these may present with thin, sharp, fractured, or incompletely healed bone. Patients that require re-contouring of bone and tissue, especially sub-gingivally, are generally not candidates for flapless placement.
In edentulous cases, a dentist must consider additional factors such as the height of the intended abutments and prosthesis. If the patient requires an alveolar ridge reduction to accommodate the restoration, a flapless procedure is contraindicated. A flapless procedure may also be contraindicated in edentulous patients whose ridges present with significant undercuts or thin, sharp, undesirable topography. If the patient requires bone grafting or augmentation procedures to correct the ridge, a flapless procedure is contraindicated.
Q. What is the proper technique to lay a flap?
There are several techniques or flap designs. I have used the mid-crestal incision with a full-thickness mucoperiosteal flap design in the vast majority of my cases.
To lay this type of flap, start with a horizontal incision along the crest of the ridge, and then extend halfway* around the buccal and lingual aspects of the adjacent teeth.

You may then carry the releasing incision on an oblique angle, towards the buccal and lingual aspects, and past the proposed implant location. Ensure the periosteum is completely severed before continuing; make additional passes over the initial incision if necessary.
Once the periosteum is completely severed from the bone, use the pointed end of a Woodson at the bone-level to begin to raise the gingival tissue. Reverse the Woodson and use the angled end to fully reflect the buccal and lingual flaps. Ensure your flaps are sufficiently elevated for ease of closure.
Hold the flap with a retractor resting on intact bone to prevent tension. When handling the flap, be cautious not to tear, pinch, or otherwise stress the tissue.

Caution: Edentulous patients tend to present with a lack of gingiva, and very fibrous quality to the tissues. These conditions may cause difficulty, and dentists must take care to avoid potential tearing when elevating the flap.
Flap Geometry:
- The width of the flap’s base should be wider* than the buccal/lingual height of the releasing incision(s). If a major artery if present in the base, this guideline is more flexible.
- The releasing incisions (sides of the flap) should either be parallel, or converge from base to apex.
- Design the flap so that the edges will not fold, and so that the retractors will not stretch or buckle the gingival tissue upon flap reflection.
*Ideally, the base should be twice as wide, as the releasing incision(s) is tall.
Flap Design Best Practices:
- Avoid incisions over bony prominences/prominent roots (ex. Canine eminence).
- Never split a papilla, especially in the esthetic region. If in doubt, make a long incision and elevate the entire papilla.
- Do not make incisions over fractured or incompletely healed bone.
- Avoid incisions over the facial aspect midcrown.
- Avoid vertical incisions near the mental foramen.
- Avoid lingual releasing incisions in the posterior mandible.
- Avoid vertical releasing incisions in the posterior palate.
- Always try to preserve axial blood supply in the base of the flap.
Surgical Tips:
- Prepare the site with local anesthetic with epinephrine.
- Always incise perpendicular to the epithelial surface (easier suturing, decreases necrosis).
- Scalpels and elevators must be sharp. I recommend using a 15, 15c, or 12b scalpel to make the incision.
- Work quickly, but carefully. Quicker procedures cause less trauma and less chance of perforation.
- Gently handle the flap’s edges, do not place the flap under tension. Do not pinch the tissues.
- If concerned about potential tissue tearing, extend the incision. A long, straight incision with adequate flap reflection will heal more rapidly than a short, torn incision.
- Adequate hemostasis is crucial to avoiding a hematoma. Achieve hemostasis with by applying pressure and packing with gauze or cotton- never wipe. Cauterize stubborn vessels if necessary.